Suggested
12 Best Document Data Extraction Software in 2025 (Paid & Free)
Health insurance claim forms are the lifeblood of accurate billing and reimbursement, yet extracting valuable data from them can be complex. These forms contain a wealth of information, including patient details, medical history, treatment specifics, and associated costs.
However, the often complex layout and mix of standardized and free-text data present challenges for traditional data extraction methods.
This guide will discuss how to extract data from health insurance claim forms.
Health insurance claim forms are standard documents used by healthcare providers. They contain the necessary patient and treatment information and help request payment from health insurance companies.
These forms contain details such as:
The most used health insurance claim forms in the US are:

Health insurance claim forms are vital for billing and claims processing systems. They provide clear communication regarding medical services' type, scope, and cost. Healthcare providers use them to get reimbursed accurately and promptly. For insurance companies, the data helps in fraud detection, claim processing, and reimbursements.
Health insurance claim forms include the following key sections:
The data extracted helps bill the insurance company for the treatment, ensure proper reimbursement for healthcare service providers, identify fraudulent activities, and prevent errors leading to claim denials. The data also impacts decisions related to patient care management and cost control.
The data from health insurance claim forms helps speed up the reimbursement process. It is also helpful for insurance companies in assessing and managing claims.
The essential data points extracted from health insurance claim forms are:
Some demographic details help prevent errors and expedite claims processing. Errors in patient information can delay reimbursement. Patient demographics can reveal significant trends and insights for population health management.
It includes:
Provider details help insurance companies verify the qualifications of the healthcare professional. They can also cross-check that the treatment was done in an authorized facility and verify the provider's area of specialization. This helps in fraud prevention and quality assurance in healthcare.
It includes:
Industry-recognized codes are standards for categorizing treatments and services. They ensure effective communication between providers and insurance companies.
Correct codes help with accurate billing, efficient claims processing, and effective healthcare analytics. Insurance companies can use them to check the appropriateness of the care provided, calculate reimbursements, and conduct health services research.
It includes:
Billing details are crucial for healthcare providers and insurance companies. The data ensures that healthcare providers are reimbursed correctly for their services, and insurance companies can use it to verify coverage and expedite reimbursement.
Accurate financial information helps prevent billing errors and claim denials and facilitates smoother cash flow between all parties involved.
It includes:
Efficient data extraction from claim forms is necessary for transforming healthcare service delivery. Swift and accurate data extraction makes the billing processes smoother. It helps enhance patient care by reducing the time taken for reimbursement. Patients receive the best care without unnecessary delays.
For insurance companies, precise data extraction aids in quickly processing claims. Correct data helps minimize errors and prevent fraud. Faster payouts help boost trust between patients, healthcare providers, and insurers.
Enhanced data extraction processes make data readily available for analyzing trends. These insights help improve patient care outcomes through informed decisions.
Data extracted from health insurance claim forms includes
It helps ensure billing accuracy to minimize claim rejections and denials. Speeding up the reimbursement process helps improve patient care. For insurance companies, precise data helps validate claims quickly. They can ensure that payouts align with the services rendered. Maintaining high accuracy in billing builds trust between patients, healthcare providers, and insurers.
Data from insurance claim forms ensures compliance with industry laws. Accurate documentation facilitates audit readiness for compliance with
Healthcare practices can prevent legal issues by protecting patient information.
Effective data extraction from claim forms improves process efficiency. This supports faster billing cycles, reduces administrative burdens, and minimizes errors. By automating administrative tasks, healthcare providers can focus more on patient care.
For insurance companies, data from healthcare claim forms helps eliminate bottlenecks. Operational efficiency helps make the healthcare system more responsive.
Data from claim forms offers invaluable insights. These enable healthcare providers to understand patient needs and tailor services better accordingly. Analytics can highlight trends in healthcare services for insurance companies. It aids in managing policy offerings and fraud detection.
The process of extracting data from health insurance claim forms is daunting. Several challenges can hinder efficiently extracting accurate data. Some key challenges include:
Successful data extraction processes require well-organized documents and claim form pre-processing. Optimizing documents before extraction increases accuracy, efficiency, and error reduction.
The following steps can help in effectively preparing health insurance claim forms:
Digitizing claim forms is the first step toward efficient data extraction. Scanning paper documents into electronic formats facilitates easy storage and retrieval. It minimizes the risk of physical damage or loss.
Ensuring the quality of the data captured is critical for accurate and efficient extraction. Data validation before extraction, provided with predefined entry options, can reduce human error.
Standardizing the data to be extracted minimizes errors during the extraction process. Healthcare providers and insurers must agree upon a consistent format for data entry. It will ensure the extraction of accurate and useful data.
Advanced OCR technology can accurately extract data from handwritten and printed text. At the same time, AI-powered tools can extract data based on context. Picking the right tool for your needs reduces errors and speeds up the process.
Health insurance claim forms are complex documents. They need careful handling to extract accurate data. The process involves identifying and retrieving specific information from the claim form. Manual methods and legacy software are time-consuming and prone to errors.
The following step-by-step guide can help ensure efficient and precise extraction:
A high-quality data extraction tool eliminates manual errors, decreases processing time, and supports faster reimbursement cycles. You must pick a tool designed for the healthcare industry. It must follow regulations and be capable of handling large volumes of forms.
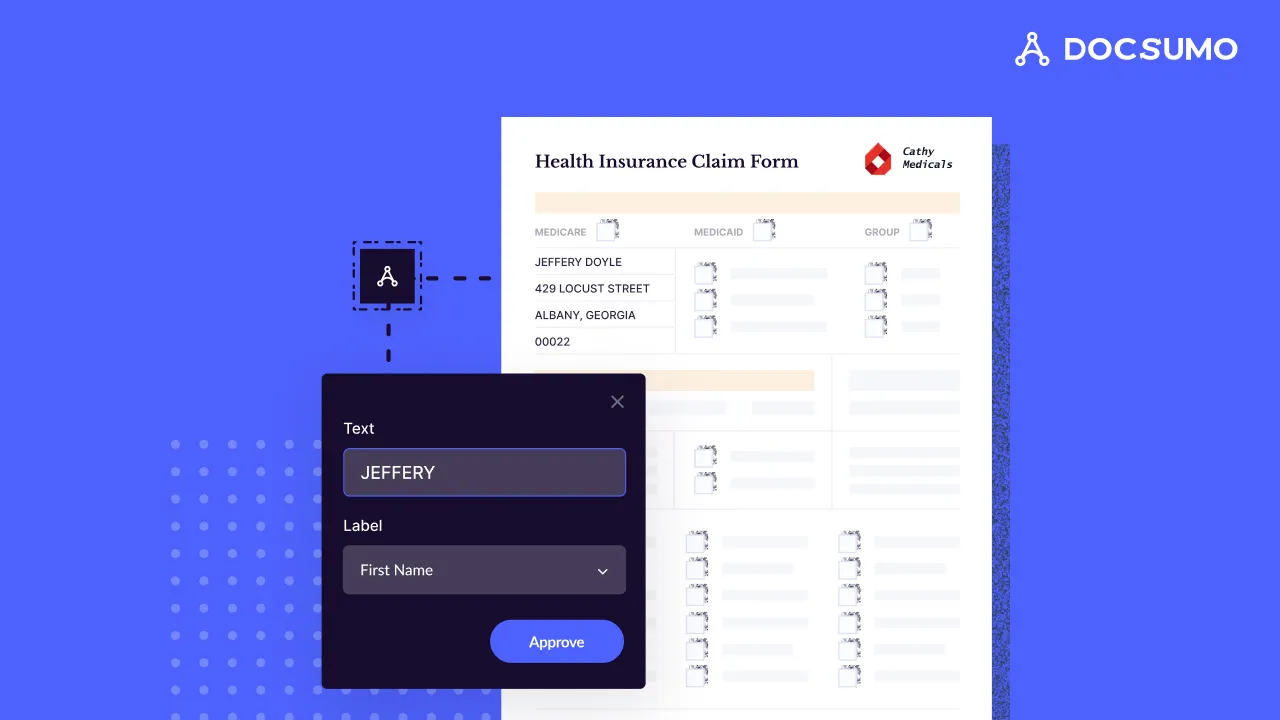
Here, we will consider Docsumo as an example of a data extraction tool. It is an advanced solution for document processing that uses OCR and AI.

On the Docsumo website, navigate to the ‘Request Trial Account’ button. The sign-up form will open. To initiate a demo request, provide your name, email ID, contact number, and document type.
Once you access your trial account, you can start uploading your claim forms. Docsumo allows you to upload documents in bulk in various formats, such as PDF, JPG, and TIF.
On the left panel, you can upload files individually or in a batch based on your workflow. Docsumo allows you to organize your documents and quickly access them. You can sort them into folders or categorize them using labels.
Select the data fields you want to extract from the claim forms. Docsumo offers a pre-defined set of data fields that you can use to initiate extraction.
You can customize extraction settings and set up custom rules for your requirements. The platform also allows you to train the AI model to extract claim forms in the future.
You can review and fix the outputs to ensure the accuracy of the claim form information. This will also train your tool for future use. You can export the extracted data from your claim forms in formats like CSV or Excel. Docsumo also supports seamless data transfer through integration with other software systems.
Advanced OCR and AI technology automate the document extraction process, which is helpful as you scale and the volume of health claim forms grows. Docsumo can extract data from large volumes of claim forms at scale. It takes a fraction of the time required by manual methods, significantly reducing errors and improving efficiency.
Use the extracted data in your claim processing and healthcare services workflow. Integrating the data through APIs with software systems like EHR, RCM, or HIS ensures hassle-free data transfer and helps automate billing and claim processing.
The data extracted from health insurance claim forms is sensitive patient information. You must ensure secure handling of the information.
Here are some best practices to follow while managing extracted data:
A data extraction tool improves healthcare operations. It reduces manual errors, increases efficiency, and accelerates reimbursement cycles. AI-powered tools address the challenges related to processing health insurance claim forms.
Docsumo is a modern tool AI-OCR-driven tool that transforms healthcare document processing. It helps insurance professionals and healthcare providers manage claim forms with 99% accuracy. Docsumo accelerates processing times for large volumes of documents by automating data extraction. It ensures faster reimbursements and improves the overall efficiency of claim processing.
Try Docsumo to automate the processing of health insurance claim forms.
Yes, AI-OCR-powered tools can accurately extract information from claim forms. After the model is trained, they do not require manual input.
Recheck the input data and retrain the AI-OCR tool to extract data correctly. After providing custom inputs to the model, you can verify the output.
Digital files and AI-OCR tools eliminate human errors. You must also double-check the outputs to ensure accuracy.