OCR for Claims Processing: How OCR Simplifies Data Extraction from Claims Documents
Efficient claims processing is crucial for industries like healthcare, insurance, finance, and legal services, where managing large volumes of data accurately and quickly is non-negotiable.
%20in%20Claims%20Processing.webp)
From ensuring compliance with stringent regulations to delivering timely claim resolutions, the stakes are high. This is where Optical Character Recognition (OCR) technology steps in, revolutionizing the way data is extracted and processed from claims documents.
OCR automates the conversion of scanned images, PDFs, and other documents into editable, searchable data. By eliminating manual data entry, OCR streamlines workflows, reduces errors, and accelerates claims processing. This not only cuts operational costs but also enhances customer satisfaction by delivering faster, more accurate claim resolutions.
In this blog, we’ll explore how OCR transforms claims processing, its key benefits like accuracy, efficiency, cost savings, and improved customer experience, and the impact it has across various industries. Let’s get in to see how OCR is shaping the future of claims processing.
What is OCR in Claims Processing?
In claims data management, OCR (Optical Character Recognition) technology automates text extraction from scanned claim documents. It converts characters from images into machine-readable text, enhancing data accuracy and speeding up processing by reducing manual entry errors. This helps insurance companies improve efficiency and claimant satisfaction.
When handling claims, OCR can process different types of documents, like financial statements, medical records, and insurance claim forms, to accurately record and convert all important information into digital form.
With a grasp of OCR technology, we can now get into how this powerful tool plays a crucial role in streamlining claims processing operations.
The Role of OCR in Claims Processing
Optical Character Recognition (OCR) technology has emerged as a critical tool in modernizing and streamlining claims processing. Let’s learn about it in detail.
- Facilitating Digitization and Organization: Optical Character Recognition (OCR) technology is key in claims processing. It turns physical documents into digital files, including insurance claims, medical records, and financial statements. This step simplifies data management, making storing, finding, and processing claims easier. As a result, operational efficiency improves.
- Extracting Relevant Information: One of the primary roles of OCR in claims processing is extracting relevant information from various documents. OCR software scans documents. Next, it identifies key data and converts it into machine-readable text. The data includes policy numbers, claimant information, dates, and amounts, which are crucial for accurate claims processing.
- Automating Repetitive Tasks: OCR technology automates many repetitive tasks. These tasks are part of claims processing, like data entry and document sorting. Traditionally, these tasks take a lot of manual effort and are often subject to human error. OCR automates these processes, saving a lot of time and money. OCR eliminates manual data entry. It reduces errors and speeds up processing. It also frees employees to focus on more important tasks.
- Ensuring Compliance with Regulatory Requirements: Compliance with rules is key in processing claims. OCR ensures claims are handled and stored correctly, following industry rules. It organizes data, aiding audits and checks. This step reduces legal risks and boosts the organization's credibility in Claims Processing.
Let's examine the significant advantages that OCR technology delivers within the claims processing domain.
Benefits of OCR in Claims Processing
Optical Character Recognition (OCR) technology greatly improves claims processing. It transforms data management.
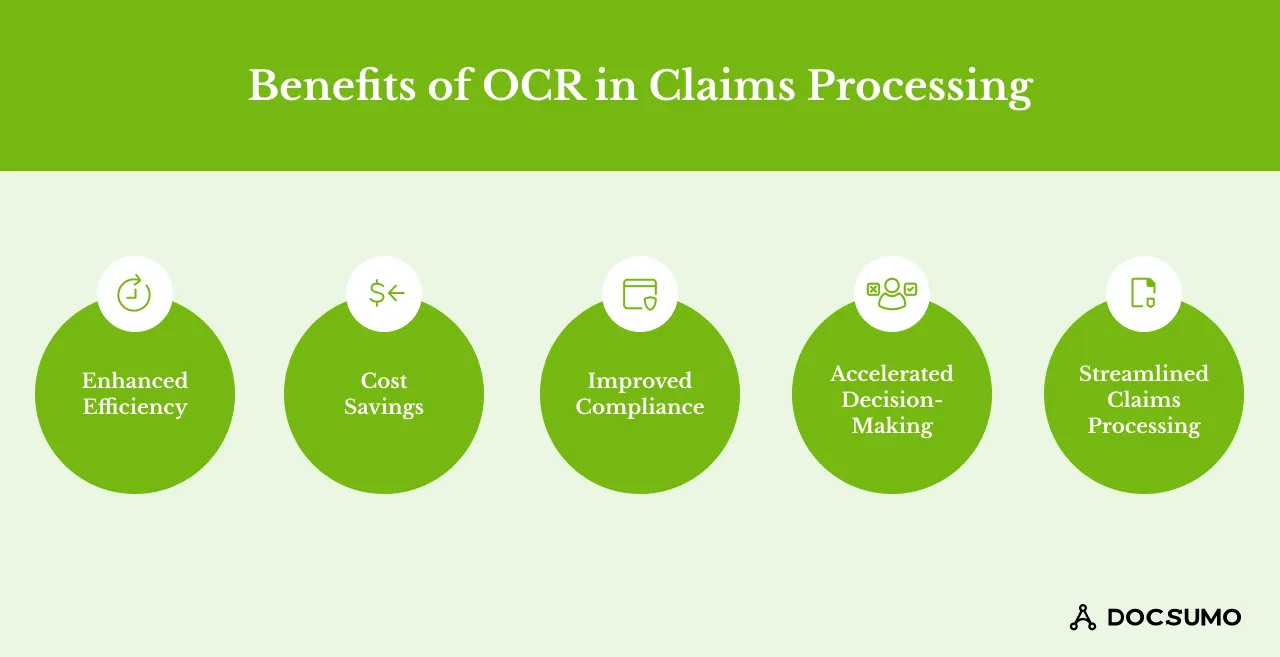
Here are its key benefits:
1. Enhanced Efficiency
OCR technology greatly speeds up claims processing. This software automates data extraction from physical documents, helping process claims faster and allowing us to handle more claims using the same resources. By reducing the need for manual data entry, OCR ensures data is processed swiftly and accurately, enhancing our workflow efficiency and accuracy.
2. Cost Savings
OCR technology automates repetitive tasks like data entry and sorting, cutting costs. Businesses can shift resources to more strategic tasks by reducing manual data processing. Moreover, it lowers errors and speeds up processes, reducing correction and delay costs and boosting financial efficiency.
3. Improved Compliance
Compliance with industry regulations and standards is crucial in claims processing. OCR technology ensures that all data is accurately captured and stored in a structured format, making audits and checks easier. By keeping accurate records, organizations can better follow the law and reduce the risk of penalties or fines for not following the law.
4. Accelerated Decision-making
OCR processes data quickly, allowing for faster claims decisions. It quickly turns physical documents into digital formats and extracts important information, enabling claims to be reviewed and approved more rapidly. This acceleration in decision-making enhances customer satisfaction by providing timely responses to claims.
5. Streamlined Claims Processing
OCR automates claim processing. It extracts, validates, and categorizes data, cutting bottlenecks and smoothing claim flow. Automated workflows enhance consistency and reliability, boosting overall performance.
Challenges of Using OCR in Claims Processing
While OCR offers significant advantages, several challenges must be considered for successful implementation and optimal performance in claims processing. Let’s evaluate them in detail.
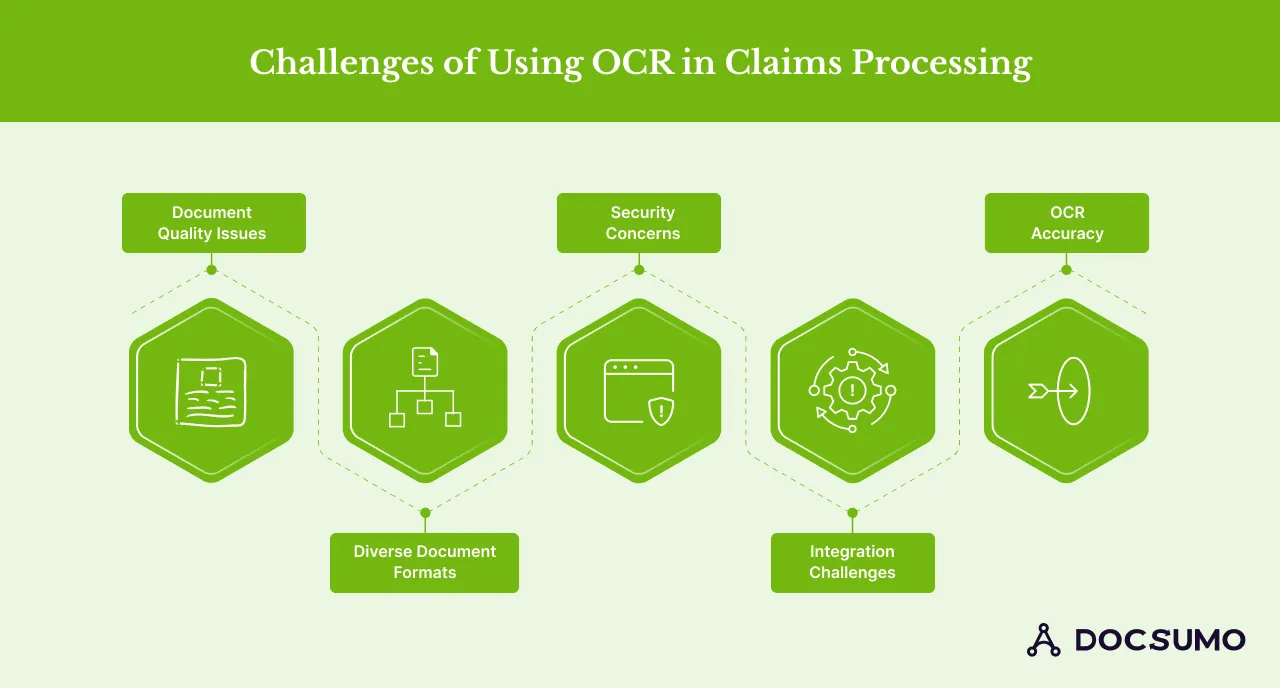
1. Document Quality Issues
Using OCR in claims processing is a big challenge. It's the quality of the scanned documents. Poor-quality documents have smudges, low resolution, or handwriting, which can lead to inaccurate data extraction. Ensuring high-quality scans is essential for optimal OCR performance.
2. Diverse Document Formats
Claims processing includes paper forms, PDFs, and images. OCR technology must adapt to various formats and layouts. This change can make data extraction harder. Using standard document formats can help fix this.
3. Security Concerns
Whenever sensitive claims data is handled, security comes first. We take precautions to collect data safely. We also make sure it's safely transferred and kept. In this manner, we can stop data breaches and prevent unauthorized individuals from accessing your information. By implementing strong security measures, we can safeguard your sensitive information.
4. Integration Challenges
Integrating OCR technology with existing claims processing systems can be complex. Addressing compatibility issues and the need for customization may present some challenges. Achieving seamless integration demands thoughtful planning and the appropriate technical know-how.
5. OCR Accuracy
OCR technology has improved greatly, but getting high accuracy is still difficult. This is especially true with complex documents or poor scans. Continuous improvement in OCR algorithms and regular system updates are necessary to enhance accuracy and reliability.
Despite these challenges, OCR technology finds valuable applications across a wide spectrum of claims processing scenarios. Let’s understand them in detail.
Use cases for OCR in Claims Processing
OCR technology is changing claims processing. It does this across many sectors by automating data extraction. It also improves efficiency. Here are some key use cases:
1. Health Insurance Claims Processing
OCR technology is vital in health insurance claims processing. It automates data extraction from medical records. It also does this from insurance claim forms and other healthcare documents. This saves time, reduces errors, and speeds up claim processing. OCR technology efficiently converts handwritten and printed documents into digital formats. It ensures that insurance claims are processed quickly and precisely. This leads to faster reimbursements and happier patients.
2. Automotive Insurance Claims Processing
In the car insurance industry, OCR technology simplifies claims. It makes them for vehicle damage and accidents. It quickly extracts details from documents like accident reports and repair invoices. This speeds up the process. With OCR, insurers can swiftly evaluate damage, assign fault, and process payments. This improves customer satisfaction and cuts processing times.
3. Property and Casualty Insurance Claims Processing
Property and casualty insurers widely use OCR to handle claims for property damage, natural disasters, and other incidents. OCR digitizes and organizes data from claim forms, property assessments, and damage reports, streamlining claim processing and leading to claim resolution faster. It also improves resource management during busy periods, like after natural disasters.
4. Workers' Compensation Claims Processing
In workers' compensation, OCR technology simplifies claim processing. It extracts data from medical records, employment documents, and injury reports, ensuring accurate capture, timely payments, and compliance. Additionally, OCR reduces administrative work and speeds up claims, benefiting employers and employees.
OCRs have various advantages. OCR technology can automate and streamline data extraction. It works across various types of claims processing, greatly enhancing efficiency, cutting costs, and improving accuracy.
To fully understand the impact of OCR, let's briefly review the typical steps involved in the insurance claims processing workflow.
Steps Involved in Insurance Claim Processing
Insurance claims processing follows a five-step process that leads up to the filing and resolution of claims. Professionals need to prepare the required documents (invoices, receipts, proof of insurance claim ownership, etc.) and gather evidence of the damages incurred in order to get approved for the claim.
Here’s how it works:-
1. Contacting Your Broker
The first step is getting in touch with your broker and forwarding them the collected information. You need to give the details needed and present evidence which will support filing your claim. Once the broker receives this, he will follow up with a claims adjuster to initiate the investigation process
2. Claim Investigation Begins
The claim investigation starts when the insurance claims adjuster looks into the matter and sees the extent of damages incurred. He/she will identify liable parties and assess how much coverage your insurance policy provides for the damages. This is the step where you can bring witnesses for investigation and get them to support you with additional evidence.
3. Policy Review
When the investigation takes place, the insurance policy gets reviewed. You will find out what won’t be covered by your policy and any deductibles you have to pay
4. Damage Assessment
The insurance adjuster may hire engineers, contractors, and appraisers to examine the extent of the damage further. Your adjuster may recommend a list of professionals to hire for making repairs, which could help you save money during the claims filing process
5. Processing of Payments
After a thorough assessment is done, if your adjuster is convinced, he/she will process your insurance claim application and proceed with payments. The damaged items will be replaced and any repairs will be carried out too. You will be contacted again during the settlement of your claim. The time taken to process your payments for the repairs or replacements will depend on a case-by-case basis on the level of severity.
The insurance claims automation process starts by incorporating data extraction technology for the review and analysis of documents used for filing claims. You can make the process go faster and speed up resolutions by transmitting information electronically via email and other online channels.
The way to do this is by leveraging technology such as Robotic Process Automation (RPA), reducing data redundancy through intelligent document processing, and finally, updating legacy systems.
Understanding the range of data extractable via OCR is crucial. Let's explore the diverse information that can be gleaned from claims documents.
Different Types of Data that can be Extracted From Claims Documents using OCR
In the claims processing industry, optical character recognition (OCR) technology is revolutionary because it can consistently and swiftly extract a wide range of crucial data from various documents. This section describes the many types of data that OCR may efficiently obtain, expediting the process and providing more accuracy and compliance.
1. Policyholder Information
The policyholder's details, including full names, addresses, phone numbers, and policy numbers, constitute the foundation of every claims document. By reliably extracting essential facts from claims forms and other relevant documents, OCR technology reduces the possibility of errors by guaranteeing that claims are associated with the correct policyholder.
2. Claim Details (Dates, Amounts, Descriptions)
Claim details are essential for processing and validating claims. OCR can effectively extract crucial data such as claim submission dates, claim amounts, and detailed descriptions of the claim. This precision helps in faster claim reviews and approvals, facilitating a streamlined workflow.
3. Medical Records and Diagnosis Codes
Since OCR retrieves data from medical records, including diagnosis codes, dates of treatment, and patient information, it is crucial to the processing of healthcare claims. This function helps ensure that claims are processed accurately in line with the medical services provided, which speeds up the reimbursement process and reduces discrepancies.
4. Information (Make, Model, VIN)
OCR may extract detailed car information, such as the brand, model, and vehicle Identification Number (VIN), for auto insurance claims. This information is essential to correctly evaluate claims for accidents or car damage and ensure that the claims processing is in line with the particulars of the vehicle in question.
5. Property Details (Location, Damage Description)
OCR technology can record important information, such as the property's location and thorough descriptions of the damage, in property insurance claims. Insurance companies need this information to evaluate the degree of damage and handle claims appropriately. This is especially true for claims arising from accidents or natural disasters.
Extracting these many kinds of data via OCR makes claims processing more accurate, compliant, and efficient. Facilitating speedier resolutions to claims increases customer happiness and speeds up claims processing.
Now that we understand the types of data that can be extracted let's explore the practical steps involved in extracting data from claims documents using OCR.
How to Extract Data from Claims Documents Using OCR
Using OCR software to extract data from claims documents involves several key steps. Here is a step-by-step guide to streamline the process:
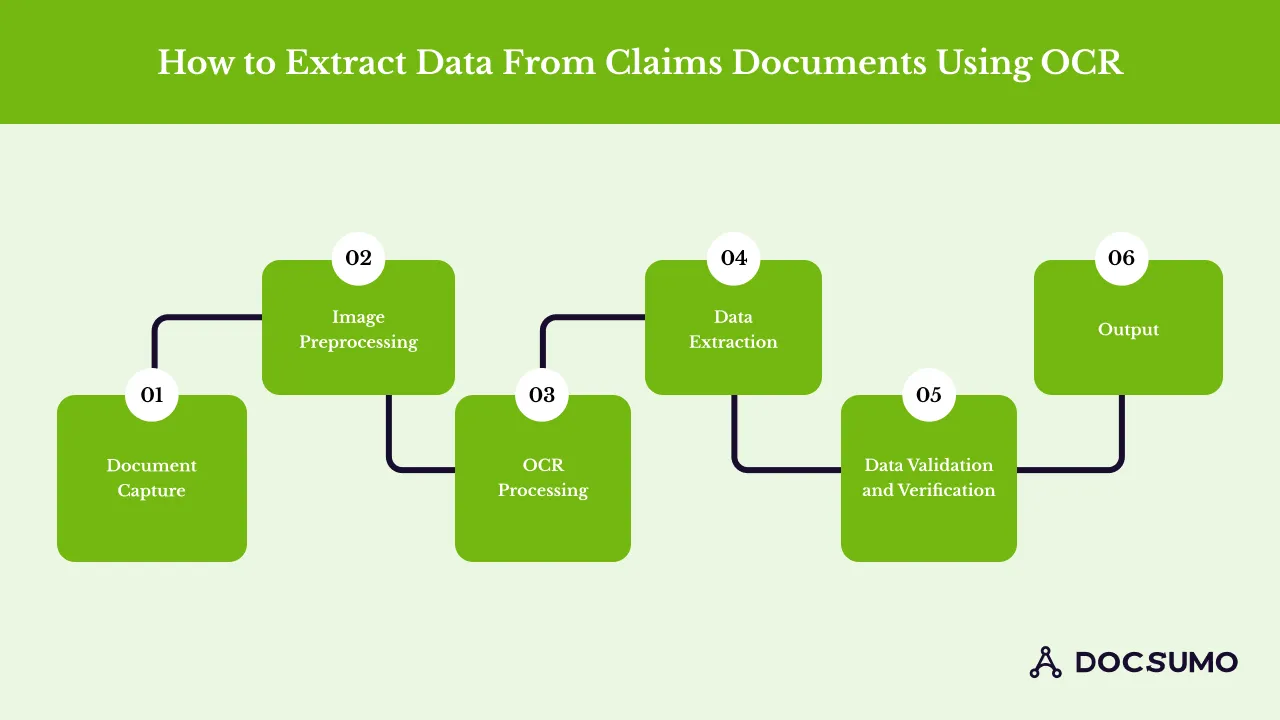
Step 1: Document Capture
The first step is capturing the physical or digital documents. This can be done either by scanning paper documents using a high-resolution scanner or by uploading existing digital images to the OCR system. The quality of these images is critical as clear, high-resolution images significantly increase the accuracy of text recognition.
Step 2: Image Preprocessing
Before OCR processing, images undergo several preprocessing techniques to improve readability for OCR algorithms.
Key steps include:
- Resolution Enhancement: Increase the DPI (dots per inch) setting to sharpen text details.
- Noise Reduction: Apply filters to remove background noise and artifacts that can obscure characters.
- Contrast Adjustment: Enhance contrast to make text stand out more clearly from the background.
- Deskewing and Despeckling: Correct any alignment issues and remove small specks on the document.
Step 3: OCR Processing
The OCR software analyzes the preprocessed images to detect and recognize text. It converts the text from images into machine-readable formats. OCR technology has evolved to recognize a wide range of fonts and handwriting, although the latter can still be challenging and may require specialized OCR solutions.
Step 4: Data Extraction
After recognizing text, the OCR software extracts key data from documents. This includes names, dates, policy numbers, and other crucial details for processing claims.
Step 5: Data Validation and Verification
After data extraction, the extracted data must be validated and verified for accuracy.
The steps involve:
- Rule-Based Validation: Apply specific rules (e.g., valid date ranges, policy number formats) to ensure the data conforms to expected formats.
- Cross-Verification: Cross-check extracted data with other databases or systems to verify accuracy. This could involve matching names with policy databases or checking codes against medical billing standards.
Step 6: Output
Finally, the validated data is put into a structured format, like JSON or XML. It can then be easily added to claims systems. This structured data facilitates automated workflows and further processing of the claims.
Docsumo: The Best OCR Software for Claims Processing Data Extraction
Docsumo stands out as a leading OCR software solution for automating claims processing. It is designed to handle the complexities of data extraction from various document formats and uses advanced OCR technology to streamline and improve claims processing workflows.
Overview of Docsumo's Features
Docsumo offers many features. They make it ideal for claims processing and data extraction. Let's have a look at them:
- Advanced data extraction capabilities: Docsumo accurately extracts data from various documents, including handwritten forms, printed materials, and digital PDFs. Its advanced algorithms boost accuracy in text recognition and data extraction, reducing errors and eliminating the need for manual corrections.
- Seamless integration options: Docsumo has strong integration capabilities. It allows seamless integration with existing claims systems, databases, and other business apps, ensuring that extracted data can be easily utilized in automated workflows.
- User-friendly interface: The software has a simple and user-friendly interface, which makes it easy for users with any technical background to access. Its dashboard allows for easy OCR process management and monitoring, ensuring smooth and efficient operation.
Why is Docsumo the best OCR software for claims processing?
Docsumo excels in claims processing data extraction for several reasons:
- High accuracy: Docsumo has state-of-the-art OCR technology. It ensures high accuracy in data extraction. It minimizes errors and ensures reliable data for claims processing.
- Scalability: Docsumo can handle large volumes of documents well. It is for groups of all sizes. It ensures that all data is stored and used legally. It follows industry rules, reducing the risk of legal issues.
- Customization: Docsumo offers customizable extraction templates and workflows. They let organizations tailor the software to their needs.
Experience better accuracy and lower costs with our top-tier OCR software. Simplify your operations and increase productivity with our user-friendly system. See how Docsumo can benefit your organization.
Book a demo today!
Frequently Asked Questions
How does OCR improve accuracy in claims processing?
OCR enhances accuracy in claims processing by automating data extraction from scanned documents, PDFs, and images, using advanced algorithms to accurately read and convert printed or handwritten text into digital data, minimizing errors from manual entry, while also incorporating validation mechanisms to cross-check extracted information against predefined rules and efficiently handling complex document formats like insurance forms or medical records, ensuring higher precision, reduced rework, and improved compliance.
What types of documents can OCR process in claims management?
OCR can handle various documents, including insurance forms, medical records, and financial statements. It processes both handwritten and printed text. OCR converts these documents into digital formats for easy editing and searching
How does OCR technology handle different document formats?
OCR systems are designed to adapt to various document formats and layouts. They can process paper forms, PDFs, and images. By standardizing document formats, OCR ensures accurate data extraction.
How does OCR ensure data security in claims processing?
OCR technology includes strong security measures to protect sensitive data. It ensures data is safely captured, transferred, and stored. These measures prevent unauthorized access and data breaches.
How does OCR technology handle handwritten documents in claims processing?
Advanced OCR systems can recognize and process various handwriting styles. They convert handwritten text into machine-readable formats accurately. This is particularly useful for processing handwritten claims forms and medical records.




.webp)
.webp)
.webp)
.webp)